Fungal acne
Encuentre un dermatólogoFungal acne happens when yeast is trapped in your skin’s hair follicles. This causes a fungal infection that appears as itchy, red or pus-filled bumps on your skin.
Unlike fungal acne, common acne usually isn’t itchy. If you believe you have a fungal acne breakout, see a dermatologist for an accurate diagnosis. The treatments for fungal acne are different from those for regular acne, and usually require antifungal medications.
What is fungal acne?
Fungal acne infections, also known as Malassezia folliculitis, are caused by Malassezia yeast. Malassezia folliculitis is also called pitryosporum folliculitis. Folliculitis is an inflammation or infection of the hair follicles.
Malassezia yeast is one of the many microorganisms (flora) that naturally occur on your skin. When in balance, your body’s flora – including bacteria, viruses and fungi – contribute to a healthy skin microbiome. When this balance is disrupted, you can have an overgrowth of Malassezia yeast.
How do I know if my acne is fungal?
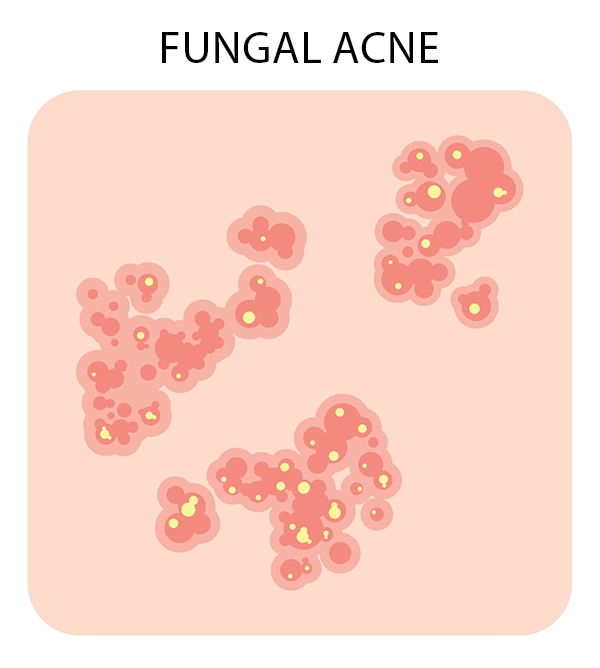
Fungal acne symptoms appear as small clusters of red or pink bumps on the skin, often resembling a rash. Some bumps may turn into whiteheads.
While fungal acne can be confused with regular acne, certain symptoms can help distinguish it. Look for the following symptoms of fungal acne:
- Clusters of small red or pink pimples that resemble a rash
- Itchy or burning pimples
- Pimples may have a red ring around them
- Pus-filled whiteheads (closed comedown)
It’s common to develop a fungal acne infection in the areas of your skin where sweat and moisture accumulate, since yeast thrives in these conditions. These areas include your:
- Pecho
- Parte de arriba de la espalda
- Hombros
- Cuello
- Forehead
- Mentón
If you've used standard acne treatments such as salicylic acid and benzoyl peroxide without success, this could be a sign your acne might be fungal.
What causes fungal acne?
Fungal acne occurs when hair follicles are damaged, allowing Malassezia yeast to get trapped inside, or when there’s an excess of yeast that enters your follicles. Several factors can trigger this skin infection, including:
- Hot, damp skin: Heat, humidity and excessive sweating encourages the growth of yeast on your skin.
- Antibiotics: Disrupts the natural balance of yeast on your skin.
- Autoimmune disorders: If you have a weakened immune system from conditions such as celiac disease, your body has difficulty controlling the growth of yeast.
- Tight clothing: Clothing, such as active wear, that traps moisture creates a warm, moist environment where yeast thrives.
- Hair removal: Yeast may get inside your follicles if they are damaged by shaving, plucking or waxing.
- Oily skin: Excess oil (sebum) can contribute to the overgrowth of yeast.
What is the difference between bacterial acne and fungal acne?
Unlike fungal acne, bacterial acne occurs when bacteria is trapped in your hair follicles. This can lead to an infection that often appears as severe types of acne, such as cysts and nodules. Bacterial acne is more common than fungal acne.
It’s possible to have acne caused by fungus and bacteria at the same time, but they’ll require different treatments. Consulting with a dermatologist is important, especially if you have multiple different causes of acne breakouts.
Diagnosing fungal acne
A fungal acne diagnosis involves the same steps as diagnosing common acne, including discussing your medical history and a physical examination of your skin. However, to confirm the presence of Malassezia yeast, your dermatologist may perform additional tests, such as a microscopic examination or culture tests of a small skin sample, often obtained through skin scraping.
Fungal acne treatment
To treat your fungal acne, your dermatologist may include the following fungal acne treatments:
- Oral antifungals: Prescription medications such as fluconazole or itraconazole are usually the most effective, especially for more widespread and severe cases.
- Topical antifungals: Creams or lotions containing antifungal agents like ketoconazole or clotrimazole.
- Antifungal washes: Over-the-counter shampoos or body washes with antifungal ingredients like selenium sulfide or zinc pyrithione.
Fungal acne treatment at home
In addition to following your treatment plan, there are at-home remedies that may help your fungal acne heal:
- Avoid irritants and triggers, such as heat and shaving
- Keep your skin clean and dry
- Avoid scratching or touching itchy or painful skin
- Use a clean, warm compress to provide pain relief
- Avoid oily skin care products
- Limit or avoid foods that promote yeast growth, like alcohol and sugar
Remember to be patient with your treatment, as it may take some time for your fungal acne to heal. Sometimes, your fungal acne infections can be persistent. If you have repeat fungal acne breakouts, your dermatologist might recommend long-term use of antifungal medications to help manage and prevent future infections.
Encuentre un dermatólogo
Find a dermatology specialist near you.
Reciba atención
Le ayudamos a vivir bien. Podemos ayudarle en persona o en línea.